
Cavernous Hemangioma Presenting With Multiple Cranial Nerve Palsies

INTRODUCTION
Welcome to the “Neuro Nuggets” column within the Journal of Medical Optometry (JoMO)! This column aims to make neuro-ophthalmic disease more approachable by blending real-world clinical cases with evidence-based medicine. The patient in this edition’s column represents the importance of utilizing neuro-ophthalmic findings to localize intracranial pathology. Enjoy!
CASE PRESENTATION
A 76-year-old male presented to the optometry clinic for a problem-focused evaluation. The patient’s past medical history included newly diagnosed Type 2 Diabetes Mellitus, atrial fibrillation s/p prior ablation, congestive heart failure, and multiple myeloma s/p two bone marrow transplants managed with lenolidamide. The patient was admitted to the hospital due to elevated blood pressure (211/105 mmHg upon admission) and headaches. The medical team managing his case was concerned about the potential for inadequate blood pressure control to impact his ocular and visual status.
The patient presented with right upper eyelid ptosis of unclear duration or onset, as the patient was asymptomatic to this feature. He reported mixed horizontal and oblique binocular diplopia over the past 1-3 weeks. He also endorsed a vague new headache complaint that was poorly characterized.
On examination, the patient’s best-corrected visual acuity was 20/40 in each eye (later ascribed to age-related nuclear sclerotic cataracts). Pupils were isocoric in bright and dim illumination. Ocular motility evaluation revealed notable supraduction and adduction deficits in the right eye and a mild abduction deficit in the right eye (Figure 1); ductions in the left eye were normal. There was also reduced levator function in the right eye. The remainder of the cranial nerve exam was normal. Visual field testing was normal in all quadrants for each eye. The anterior segment evaluation was normal and age-appropriate in each eye. Intraocular pressure was at goal and normotensive in each eye. No abnormal optic disc abnormalities or retinal findings were present on posterior segment evaluation. The clinical presentation was concerning for a partial pupil-sparing right cranial nerve (CN) 3 palsy and mild right CN 6 palsy, raising concern for a possible right cavernous sinus lesion. The patient was given a black occluding patch to help alleviate his diplopia.
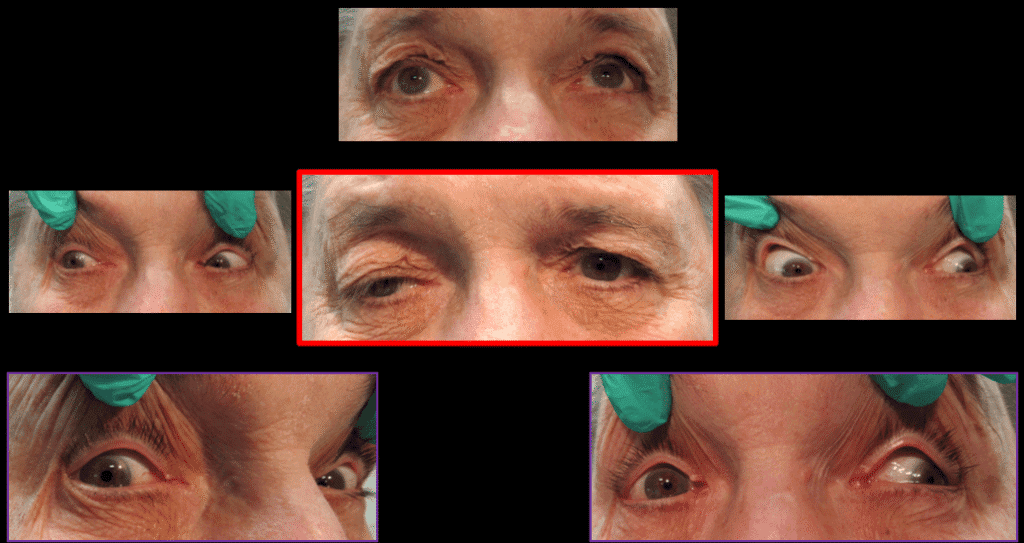
Figure 1. Ocular motility at presentation. Note limitations in abduction, adduction, and supraduction of the right eye. Also note the significant right upper eyelid ptosis and “down-and-out” posture consistent with right CN3 palsy.
Brain magnetic resonance imaging (MRI) with and without gadolinium contrast had already been obtained by the neurology team due to concern for headaches in the setting of inadequate blood pressure control, and the imaging was initially read as normal. After the eye exam, the optometry team re-evaluated the neuroimaging and identified an area of abnormal enhancement at the level of the right cavernous sinus that could potentially explain the patient’s neuro-ophthalmic presentation (Figures 2 and 3). Additional MRI sequences with thin cuts were obtained to better characterize the lesion, which measured 1-1.6 cm in size. A wide differential diagnosis was considered for the right cavernous sinus lesion, including a neoplastic process (stemming from underlying multiple myeloma), schwannoma, meningioma or hemangioma, among others.
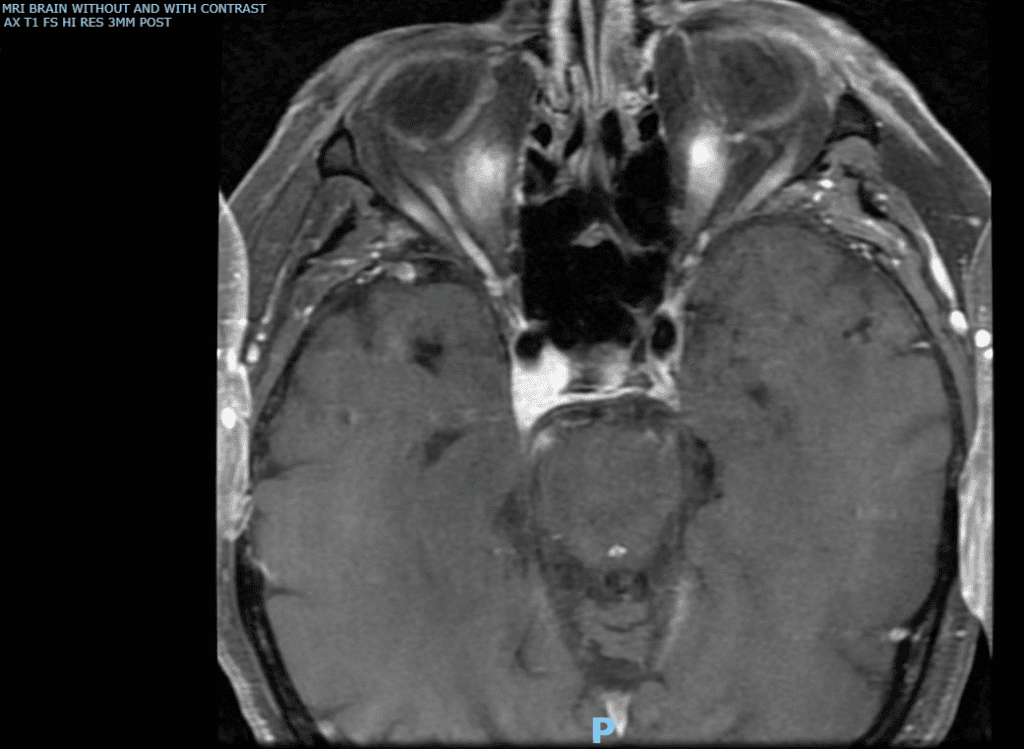
Figure 2. Brain MRI. Axial T1 high-resolution images post-contrast. Note the lesion in the right cavernous sinus with homogenous contrast enhancement.
Initially, the inter-disciplinary team’s plan was to serially monitor the cavernous sinus lesion and follow up in a few months’ time to determine growth pattern vs stability. However, the patient sustained a fall, which prompted another hospitalization at an outside facility. At that time, the patient’s neurosurgery team elected to biopsy the right cavernous sinus lesion. The biopsy of the right cavernous sinus lesion was consistent with a cavernous hemangioma. At this time, the patient is being serially evaluated to determine if any additional intervention is necessary.
DISCUSSION
Cavernous hemangiomas (also known as cavernomas, cavernous malformations, or cavernous angiomas) are rare benign intracranial vascular malformations.1-4 They have been described as “mulberry-appearing,” multi-lobulated masses often with a purple hue.2 Despite their name, cavernous hemangiomas do not exclusively present in the cavernous sinus, and, in fact, the cavernous sinus is an uncommon site of these vascular malformations.2 Cavernous hemangiomas can be characterized as intra-axial (within the cerebral parenchyma) or extra-axial (such as in the cavernous sinus).3,4 Classically, these lesions present in middle-aged women, so the patient in this report represents an atypical demographic to have this diagnosis.4 Though non-specific, the MRI features of cavernous hemangiomas often appear as hypo- or iso-intense on T1-weighted images, hyperintense on T2-weighted images, and homogeneously enhance after administration of contrast agents.4 This feature helps distinguishing these lesions from others such as schwannomas or meningiomas which may show heterogeneous contrast enhancement.4 Radiologic and clinical findings in cavernous hemangiomas are still considered non-specific, and tissue biopsy may be the only way to yield a definitive diagnosis.2
The underlying pathogenesis of cavernous hemangiomas is uncertain, but reports suggest that abnormal vascular development with genetic predisposition potentially contributing (e.g. cerebral cavernous malformation, CCM genes).2 Depending on their location, these lesions may produce symptoms (e.g. headache, cranial nerve palsy, visual loss, etc) from mass effect on surrounding structures.1 This patient presented with features of right CN 3 involvement (significant right upper eyelid ptosis, right eye adduction limitation, right eye supraduction limitation) and right CN 6 involvement (mild right abduction limitation). Both CN 3 and CN 6 course through the cavernous sinus, which helped to clinically localize pathology to this area.
A handful of case reports document cavernous hemangiomas in the cavernous sinus.1-6 Given the complex anatomy within the cavernous sinus and presence of both neural and vascular elements (i.e. internal carotid artery, CN 3, CN 4, branches of CN 5, CN 6, and sympathetic nerve fibers), eye care providers are likely to encounter disease that impacts this part of the neuroanatomy.5 Patients may present with varying types of ophthalmoplegia, ptosis, proptosis, chemosis, or trigeminal sensory loss depending on the structures impacted.5 Various types of infections, inflammatory and neoplastic processes can be found in the cavernous sinus, often creating a need for inter-disciplinary work-up and management in these cases.5,7 As in this case, radiosurgical approaches are often considered to minimize mortality and morbidity in this area, though tissue biopsy can still serve a crucial role in confirming diagnosis.2,5 Low doses of radiation treatment may be beneficial to achieve therapeutic benefit in some patients.2,5 Eye care providers should be well-versed in the various presentations of cavernous sinus pathology and prepared to manage them before and after treatment.
CLINICAL PEARLS
- Eye care providers are encouraged to review neuroimaging for patients presenting with neuro-ophthalmic signs and
- Patients with multiple cranial nerve palsies may have pathology localized to the level of the cavernous sinus.
- Cavernous hemangiomas are rare benign intracranial lesions that may produce varying clinical symptoms from impact on surrounding neuroanatomical or vascular structures.
REFERENCES
- Bozkurt OF, Kuzucu P, Sahin MM, Celtikci E. Cavernous hemangioma within the cavernous sinus: illustrative case. J Neurosurg Case Lessons. 2024 Sep 2;8(10):CASE24227. doi: 10.3171/CASE24227. PMID: 39222542; PMCID: PMC11373689.
- Hassanzadeh S, Gao L, Alvarado AM, Camarata PJ, Lakis NS, Haeri M. Extra-Axial Cavernous Angioma: A Case Report and Review of the Literature. Neurol Int. 2024 Jan 12;16(1):162-185. doi: 10.3390/neurolint16010010. PMID: 38251058; PMCID: PMC10801606.
- Ibrahim D, El Fiki A, Hafez M, Saleem S. Report of a case of cavernous haemangioma of the cavernous sinus. BJR Case Rep. 2019 Nov 15;5(4):20190031. doi: 10.1259/bjrcr.20190031. PMID: 31938563; PMCID: PMC6945263.
- Sohn CH, Kim SP, Kim IM, Lee JH, Lee HK. Characteristic MR imaging findings of cavernous hemangiomas in the cavernous sinus. AJNR Am J Neuroradiol. 2003 Jun-Jul;24(6):1148-51. PMID: 12812943; PMCID: PMC8149037.
- Nagaraja CT, Ramalingaiah AH, Arimappamagan A, Mitra S, Shukla D, Srinivas D, Krishna SS, Mahadevan A. Spectrum of Surgically Resected Lesions of the Cavernous Sinus: A Neuropathologic Audit. J Neurosci Rural Pract. 2022 Aug 7;13(3):495-509. doi: 10.1055/s-0042-1750707. PMID: 35946008; PMCID: PMC9357489.
- Wu J, Deng P, Qian J, Lu Y, Ding Z, Hu X, Gong Y, Tang X, Ma M. Endoscopic endonasal transsphenoidal surgery for unusual sellar lesions: eight cases and review of the literature. Front Neurol. 2024 Feb 13;15:1309691. doi: 10.3389/fneur.2024.1309691. PMID: 38414554; PMCID: PMC10896968.
- Kane, Joseph. Cavernous Sinus Involvement In Multiple Myeloma. The Journal of Medical Optometry. 2024 August; Vol 2, Issue 3. doi:10.62055/47099956Qn












