Letter to the Editor: Embracing Specialization in Optometric Care: A Public Health Imperative
In recent decades, the evolution of specialized care in medicine has demonstrably enhanced patient outcomes, streamlined healthcare delivery, and optimized resource allocation for both federal and governmental agencies. By following a similar model, the field of optometry can reap comparable benefits. Recognizing subspecialties such as medical optometry, pediatric and vision therapy, and low vision care not only aligns with modern trends in medical practice but also directly contributes to improved public health outcomes.
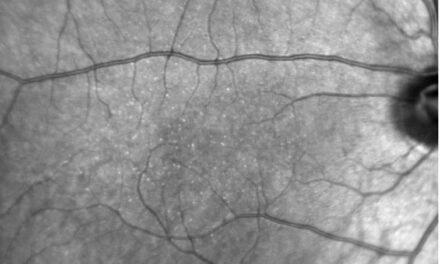
The evolution of medical specialties can be a model for optometry. Over the last 20 years, medicine has increasingly moved toward new sub-specializations. Fields like neurohospitalist, addiction medicine, clinical informatics, and sleep medicine are a few of the subspecialties that enhanced diagnostic accuracy and treatment precision, which has had a positive net effect on society and public health. In ophthalmology, the medical retina specialty has grown.
Studies have shown that specialized care reduces morbidity, shortens recovery times, and lowers long-term healthcare costs by addressing complex conditions early and efficiently.1,2
A critical component of the evolution of medical specialties is the rigorous process by which new fields are recognized and accredited. In medicine, the establishment of a new specialty typically involves demonstrating a distinct body of knowledge, a unique scope of practice, and evidence of improved patient outcomes. Regulatory agencies such as the American Board of Medical Specialties (ABMS) and the Accreditation Council for Graduate Medical Education (ACGME) in the United States oversee this process, ensuring that proposed specialties meet distinct educational and clinical criteria before being formally recognized.3 Similar protocols are observed worldwide, with national health authorities and specialty boards collaborating to maintain high standards of care and patient safety.
Development and Structure of the American Board Certification in Medical Optometry
In optometry, this rigorous process is exemplified by the American Board Certification in Medical Optometry, setting a strong foundation for establishing optometry as a recognized specialty. This board has developed a comprehensive certification pathway that includes a multi-tiered examination process, structured residency and fellowship training programs, and ongoing continuing education requirements. These measures ensure that practitioners are thoroughly trained in the diagnostic and treatment protocols for complex ocular conditions, mirroring the standards seen in medical specialties. The board’s structured approach not only bolsters clinical excellence but also reinforces the credibility and integration of specialized optometric care within the broader healthcare system.4
Medical Optometry, as a specialty, shifts the traditional optometric focus of corrective refractive care to emphasize the medical management of ocular pathology using existing evidence-based protocols. This specialization ensures that optometrists are skilled in routine eye examinations and adept at identifying early signs of systemic diseases manifesting in the eyes. Influential voices in the optometric community support this paradigm shift. The editorial “Medical Optometry: No Longer An Option,” published in the Fall 2019 issue of the American Academy of Optometry e-newsletter, is a call for specialized training as both timely and essential for advancing patient care.5
Medical optometry is not the only specialty that needs to be recognized. Pediatric optometry and vision therapy address the unique needs of children, a demographic where early intervention can have lifelong benefits. Subspecialists in this area are trained to manage amblyopia, binocular vision disorders, and learning-related visual deficits, often working closely with educators and pediatricians. Research has shown that early, targeted intervention in pediatric care can lead to significant improvements in academic performance and overall developmental outcomes.6 Recognizing pediatric optometry as a specialty underscores the critical role of vision in early childhood development, justifying further investment in training and resources.
Low vision care is another critical area where sub-specialization can make a substantial public health impact. Specialists in low vision not only provide rehabilitation services but also develop individualized strategies to maximize remaining vision, thereby improving patients’ quality of life. With an aging population and increasing prevalence of chronic diseases affecting vision, a dedicated low vision specialty could lead to better management of visual impairment, ultimately reducing the societal and economic burden of vision loss. Governmental agencies stand to benefit from such initiatives by decreasing long-term care costs and enhancing community health outcomes.7
Public Health Benefits
The recognition of specialized optometric care extends beyond patient outcomes, it represents a strategic public health investment. Specialized training leads to:
- Enhanced Collaborative Care: With clearly defined specialties, optometrists can better integrate with other healthcare professionals, fostering multidisciplinary approaches to complex health issues.
- Cost-Effective Healthcare: Early diagnosis and tailored treatment protocols reduce the incidence of severe complications, thereby lowering overall healthcare expenditures.
- Public Health Initiatives: Government agencies can design more precise public health campaigns and allocate resources more effectively when they have access to a cadre of specialized practitioners.
As healthcare continues to evolve toward more precise, patient-centered models, the case for recognizing specialized optometric care becomes increasingly compelling. Establishing subspecialties such as medical optometry, pediatric and vision therapy, and low vision care aligns with the proven benefits seen in other areas of medicine. It promises not only to enhance clinical outcomes but also to serve as a prudent public health strategy, offering significant long-term benefits for patients. By embracing specialization, optometry can join the forefront of healthcare, ensuring that targeted, effective eye care becomes an integral component of our public health framework.
References
- Smith, A., et al. (2006). The Evolution of Medical Specialties: Enhancing Patient Outcomes through Focused Expertise. Journal of Medical Specialization.
- Jones, B., et al. (2010). Specialized Care in Pediatric Medicine: A Systematic Review. Pediatrics Today.
- American Board of Medical Specialties. (2018). Standards for Recognition of New Specialties. ABMS.
- American Board Certification in Medical Optometry. (2020). Certification Standards and Process. ABCMO.
- Gonzalez, A. (2019). Medical Optometry: No Longer An Option. American Academy of Optometry E-Newsletter, Fall 2019.
- Thompson, R., & Rivera, M. (2012). Early Intervention in Pediatric Vision: Impact on Development and Learning. Journal of Pediatric Ophthalmology.
- Lee, C., et al. (2015). Cost-Effectiveness in Low Vision Rehabilitation: A Public Health Perspective. Health Affairs Journal.
Optometrist with clinical, reserch and administrative experience.