Decoding Alphabet Soup
I got a call from my sister, an MD, last night. She said that she received an optometry note which someone asked her to review but she couldn’t make heads or tails of it. As we all know, there are countless acronyms used in eye care and it can sometimes feel like trying to decode alphabet soup. We are also seeing new acronyms coming onto the scene all the time. Although the use of abbreviations and acronyms is inevitable, it is important that there is a consensus regarding the meaning of these abbreviations so we are able to effectively communicate with our colleagues. So, how do we reach a consensus?
Consensus statements are developed in an effort to address clinical issues where information is incomplete and developing, and where guidelines are lacking.1 Although there is no consensus on exactly how consensus statements are developed, they are generated by a group of experts in a specified field using a defined methodology.1 This group of experts could be a task force appointed by an organization such as the American Academy of Ophthalmology (as seen in their special report for developing novel end points for premium intraocular lens introduction) or a panel formed from members of multiple professional associations joining forces to work together (as is seen in the consensus statement on management of thyroid eye disease written by the American Thyroid Association and the European Thyroid Association).2,3 Although specific methodology does exist for creating consensus statements, such as the Delphi method and the nominal group technique (NGT), these are not always used in generating consensus statements.4 However, a thorough consensus statement will include a clear explanation of the methods that were used in generating consensus.
One contemporary example of a consensus statement in eye care is the Classification of Atrophy Report. This is a multipart report generated by a panel of experts that convened to participate in the Classification of Atrophy Meetings (CAM) in order to develop consensus terminology to define atrophy in the setting of age-related macular degeneration. The selection criteria for the panel included having a history of relevant publications in AMD, recent AMD and imaging research contributions, a track record of success in collaboration and consensus efforts and the ability to attend the CAM meetings.5 This panel was ultimately comprised of an international group of retinal specialists, retinal histologists, optical engineers and image reading center experts.5
The methodology used to reach consensus definitions was also clearly outlined in the CAM reports and is summarized here. After evaluating the advantages and disadvantages of multiple imaging modalities, OCT was defined as the base imaging method used to define atrophy. CAM co chairs then reviewed and distributed the pre-existing literature on macular degeneration that was obtained using the search terms atrophy and classification. Participants were asked to grade several image sets indicating presence or absence of atrophy and to define the margins in atrophic areas. They were also asked to identify key features in the areas of potential atrophy, such as areas of hypertransmission. These results were evaluated for areas of agreement and disagreement and this information was used as a starting point for consensus discussions.5
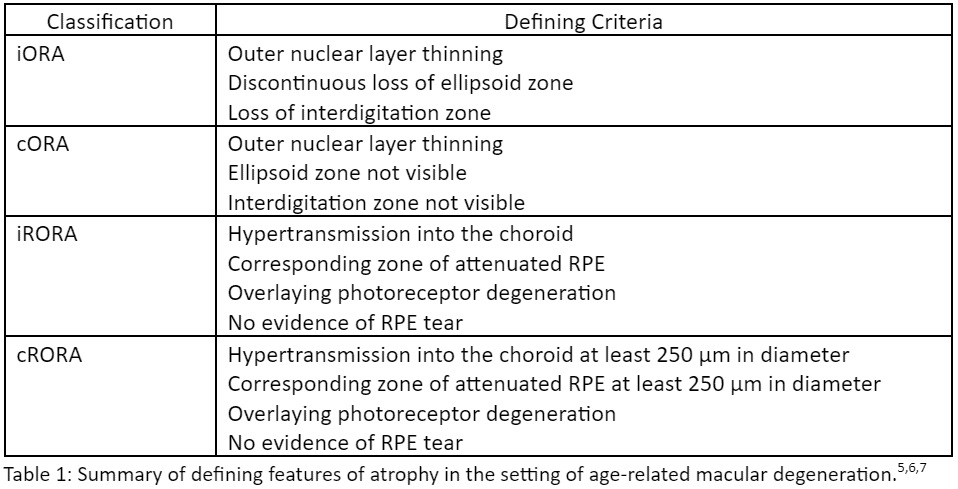
After literature review, image grading and consensus discussions, the CAM group recommended the use of four terms to describe atrophy associated with AMD. These terms are based on the specific retinal layers involved and use of four different terms recognizes the fact that atrophy is a gradual process that evolves in stages.5 The consensus terms reached by the CAM group are: complete RPE and outer retinal atrophy (cRORA), incomplete RPE and outer retinal atrophy (iRORA), complete outer retinal atrophy (cORA) and incomplete outer retinal atrophy (iORA). These terms also acknowledge the fact that outer retinal atrophy can be observed without RPE atrophy, however, the CAM participants agreed that thinning of the outer retina was observed in all cases of RPE atrophy in the setting of AMD.5
See Table 1 for the features that were used to define each term. Note that cORA has the same features as iORA but with a complete loss of the ellipsoid zone (EZ) and interdigitation zone (IZ), just as cRORA has similar features as iRORA but with additional requirements regarding the size of the lesions7. There must also be evidence of overlying photoreceptor degeneration, as described above.5 Neither of the terms iRORA or cRORA should be used when there is presence of an RPE tear.5,6
The consensus definitions and acronyms developed by the CAM group illustrate a great example of how transparency with the consensus process can aid in our understanding of how these terms were created. Having this background can improve our knowledge of the disease process as well as assist in our ability to communicate with our colleagues. Clearly defining stages of a condition can also improve our ability to identify patients that may be candidates for intervention and may also enable us to create clearer inclusion and exclusion criteria for ongoing trials. However, as diagnostic imaging and scientific knowledge continues to evolve, new ophthalmic features will undoubtedly be discovered requiring new terminology and even more acronyms. As these advances occur, we should consider whether it is necessary to use acronyms as opposed to the full terminology. With advancements in smartphrase technology in our electronic health record (EHR) systems perhaps we can move to using full terminology in our clinical notes to decode the alphabet soup for the sake of our fellow medical colleagues like my sister.
References
- Niederberger M, Spranger J. Delphi Technique in Health Sciences: A Map. Front Public Health. 2020;8:457. Published 2020 Sep 22. doi:10.3389/fpubh.2020.00457
- Lum F, Holladay JT, Glasser A, et al. Special Report: The American Academy of Ophthalmology Task Force for Developing Novel End Points for Premium Intraocular Lenses Introduction. Ophthalmology. 2017;124(1):133-134. doi:10.1016/j.ophtha.2016.09.028
- Burch HB, Perros P, Bednarczuk T, et al. Management of Thyroid Eye Disease: A Consensus Statement by the American Thyroid Association and the European Thyroid Association. Thyroid. 2022;32(12):1439-1470. doi:10.1089/thy.2022.0251
- Humphrey-Murto S, Varpio L, Wood TJ, et al. The Use of the Delphi and Other Consensus Group Methods in Medical Education Research: A Review. Acad Med. 2017;92(10):1491-1498. doi:10.1097/ACM.0000000000001812
- Sadda, Srinivas R et al. “Consensus Definition for Atrophy Associated with Age-Related Macular Degeneration on OCT: Classification of Atrophy Report 3.” Ophthalmology 125,4 (2018): 537-548. doi:10.1016/j.ophtha.2017.09.028 Sadda, Srinivas R et al. “Consensus Definition for Atrophy Associated with Age-Related Macular Degeneration on OCT: Classification of Atrophy Report 3.” Ophthalmologyvol. 125,4 (2018): 537-548. doi:10.1016/j.ophtha.2017.09.02
- Guymer, Robyn H et al. “Incomplete Retinal Pigment Epithelial and Outer Retinal Atrophy in Age-Related Macular Degeneration: Classification of Atrophy Meeting Report 4.” Ophthalmology 127,3 (2020): 394-409. doi:10.1016/j.ophtha.2019.09.035
- Spaide RF, Jaffe GJ, Sarraf D, et al. Consensus Nomenclature for Reporting Neovascular Age-Related Macular Degeneration Data: Consensus on Neovascular Age-Related Macular Degeneration Nomenclature Study Group [published correction appears in Ophthalmology. 2020 Oct;127(10):1434-1435]. Ophthalmology. 2020;127(5):616-636. doi:10.1016/j.ophtha.2019.11.004
Dr. Blake received her Doctorate of Optometry degree from UC Berkeley in 2007. From there, she went on to complete the cornea and contact lens residency program at New England College of Optometry. She had spent the majority of her career in community health prior to pursuing opportunities in medical affairs.