Peripapillary Retinoschisis in a Patient with Severe Primary Open Angle Glaucoma

Abstract
Background: Peripapillary retinoschisis is a rare finding that may be associated with the progression of primary open angle glaucoma (POAG).1 Potential pathophysiological mechanisms have been proposed to explain this association, such as acute and chronic increase in intraocular pressure, vitreopapillary traction, and Müller cell dysfunction from optic nerve head deformation. OCT imaging has revealed hyper-reflective strut-like pillars within the schisis cavity described as “bridging structures.” These structures cast a shadow onto the retina, similar to those seen with retinal blood vessels, and spacing of these pillars have been consistent with the spacing profile of Müller Cells crossing the RNFL. While peripapillary retinoschisis may spontaneously resolve, other strategies may include lowering intraocular pressure, intraocular injections, or pars plana vitrectomy.present a patient with peripapillary retinoschisis incidentally found during a workup for primary open angle glaucoma.
Case report: A 65-year-old male with large cupping and focal notching presented for a glaucoma workup, including fundus biomicroscopy, fundus photography, and optical coherence tomography (OCT). Significant findings from that exam were intraocular pressures of 29mmHg OD and 27mmHg OS, thinning of the neuroretinal rim tissue superiorly and inferiorly in both eyes on clinical exam, flagged areas of retinal nerve fiber (RNFL) and ganglion cell layer (GCL) thinning inferiorly and superiorly, and retinoschisis extending from the optic nerve towards the macula in the right eye. Latanoprost 0.005% QHS OU was initiated, a retinal specialist consult made and a follow-up IOP check was scheduled for 6 weeks.
Conclusion: This case reinforces the potential association between peripapillary retinoschisis and severe glaucoma. Several pathophysiological mechanisms have been proposed to explain the connection between these pathologies. Imaging with fundus photography and OCT should be obtained to confirm the presence of retinoschisis and document the severity of glaucoma, with treatment focused on lowering intra-ocular pressure through medical or surgical means.
Keywords: peripapillary retinoschisis, intraocular pressure, vitreopapillary traction, Müller cell dysfunction
Introduction
Peripapillary retinoschisis is a rare finding that may be associated with the progression of primary open angle glaucoma (POAG).1 Potential pathophysiological mechanisms have been proposed to explain this association, such as acute and chronic increase in intraocular pressure, vitreopapillary traction, and Müller cell dysfunction from optic nerve head deformation. OCT imaging has revealed hyper-reflective strut-like pillars within the schisis cavity described as “bridging structures.” These structures cast a shadow onto the retina, similar to those seen with retinal blood vessels, and spacing of these pillars have been consistent with the spacing profile of Müller Cells crossing the RNFL. While peripapillary retinoschisis may spontaneously resolve, other strategies may include lowering intraocular pressure, intraocular injections, or pars plana vitrectomy.
Case report
A 65-year-old Hispanic male presented for a glaucoma workup due to large cupping and focal notching identified the previous day during a problem-specific exam, in which the patient was diagnosed with a subconjunctival hemorrhage. His last comprehensive eye exam was about 15 years prior, and he denied ever being diagnosed with an ocular condition. The patient’s medical history was positive for hypercholesterolemia and mild thyroid dysfunction. He denied any significant family ocular or medical history. He had no history of tobacco, alcohol, or drug abuse and no known drug or seasonal allergies. He was oriented to time, place, and person and his mood was appropriate.
Upon examination, the patient denied any visual complaints at distance without correction, and entering visual acuity through his current glasses was recorded as 20/30+2 OD, 20/30+2 OS, and 20/25 OU.
Pupils were equal, round, and reactive to light, with a 1+ relative afferent pupillary defect OS. Confrontation field testing was full to finger counting OD, and a superior nasal constriction that respected the horizontal midline was noted OS. Extraocular motility evaluation was smooth, accurate, full, and extensive. Goldman applanation tonometry measured 29 mmHg OD and 27 mmHg OS at 3:18pm. Slit lamp biomicroscopy revealed normal adnexa, lashes, puncta, and lids with 1+ capped meibomian glands OU. The right eye had a 3+ subconjunctival hemorrhage temporally and inferior-temporally. Mild conjunctivochalasis was observed in both eyes. The right and left cornea were clear. Both anterior chambers were quiescent without evidence of cells or flare; estimations of the temporal and nasal angle were >1:1 by Van Herick OU. Both irides were flat and brown. Pupils were dilated using one drop of 1% tropicamide and one drop of 2.5% phenylephrine OU.
Evaluation of the crystalline lens revealed 1+ nuclear sclerotic cataracts OU. Fundus assessment revealed optic nerve cup-to-disc ratios of 0.80H/0.90V OD and 0.85H/0.95V OS. Both cups were deep with focal notching of rim tissue superiorly and inferiorly, with completely absent rim tissue inferiorly OS. There was no evidence of optic nerve pallor or optic pits. Evaluation of the macula revealed mild elevation extending from the optic nerve inferiorly towards the fovea OD, while the macula was flat and clear OS. The vitreous was optically clear OU. The vasculature was normal OU. Peripheral evaluation showed no breaks or tears 360 degrees in either eye.
Same day fundus photography and OCT imaging were performed, and their results can be seen in Figures 1-3.

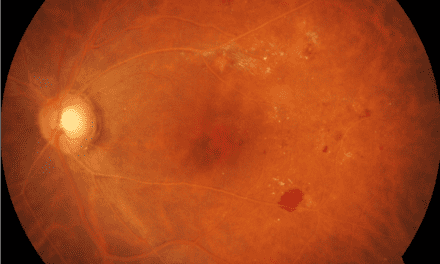
Figure 1. Fundus photography of both eyes. In the right eye, there is subtle obscuration of the retinal blood vessels extending from the inferior aspect of the optic nerve towards the macula; which appeared elevated when examining the patient binocularly. In the left eye, focal notching of the superior and inferior optic nerve can be visualized, correlating to retinal nerve fiber layer wedge defects which extend into the arcades without any retinal elevation or focal vessel obscuration.

Figure 2. 3D-Wide OCT imaging of both eyes. In the right eye, significant thickening can be visualized on the RNFL and GCL thickness heat maps, confounding the circumpapillary RNFL (cpRNFL) thickness profile map on the NSTIN curve inferiorly. In the left eye, significant thinning of the RNFL and GCL can be seen more prominently inferiorly on their respective heat maps, correlating to flagged sectors and focal thinning which is greatest inferiorly on the cpRNFL NSTIN curve.

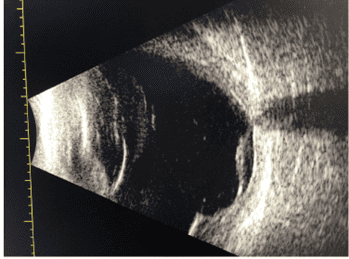
Figure 3. Raster images of the right eye. The left image reveals splitting of the ganglion cell extending from the optic nerve temporally with an intact foveal contour. The right image reveals splitting of the retina inferior to the optic nerve in the inner and outer retinal layers with a small pocket of subretinal fluid.
The patient refused visual field testing, pachymetry, and gonioscopy that day. Latanoprost 0.005% QHS OU was initiated and potential side effects of prostaglandin analogs were reviewed. The patient was educated regarding the diagnosis of POAG and the risk of further permanent vision loss if left untreated. A referral to a retina specialist was placed due to presence of subretinal fluid and the proximity of the retinoschisis to the fovea. A 6-week follow-up was scheduled with optometry for an IOP check and visual field testing.
Discussion
Peripapillary retinoschisis is a pathological splitting of retinal layers that may be associated with the progression of POAG.1 While the underlying pathophysiology of the onset and progression is not fully understood, several mechanisms have been proposed. First, the development of peripapillary retinoschisis may be preceded by an acute rise in intraocular pressure (IOP) coupled with increased optic disc cupping and subsequent accumulation of liquified vitreous in the retina. A potential association between macular retinoschisis and elevated IOP resulting from chronic angle closure has also been identified.2 Reports suggest that sustained elevation of intraocular pressure in conjunction with optic disc cupping may lead to direct interconnections with the adjacent retina and vitreous space, enabling vitreous fluid migration.3
Another proposed mechanism suggests that vitreopapillary traction may be the precipitating event of peripapillary schisis.4 Some reports have shown that RNFL thickness from peripapillary is greatest at the point of vitreal traction when measured with Optical Coherence Tomography (OCT).3–5 However, other studies have failed to present findings of vitreous traction with concurrent retinoschisis.6–10 One study involving 33 patients that exhibited some form of peripapillary retinoschisis found only one patient who presented with both vitreopapillary traction and peripapillary schsis.11 This variability in the literature may be the result of the limited ability of spectral domain OCT to accurately evaluate the vitreoretinal interface.12 Furthermore, one study did not find any significant difference in the vitreoretinal interface between glaucomatous eye with retinoschisis and those without.13 Factors such as age, gender, or axial length have been found to have a stronger correlation to posterior vitreous detachment, suggesting that vitreopapillary traction may not be the primary mechanism involved.14–20
A third mechanism which has been proposed implicates Müller cell dysfunction, which has been identified as a target of glaucomatous progression and optic nerve head deformation.21 One study evaluated twelve eyes with retinoschisis associated with a diagnosis of glaucoma or glaucoma suspect. OCT imaging revealed that all subjects exhibited “bridging structures,” which crossed the schisis axially.22 The study identified these “bridging structures” as Müller cells, which provide tensile strength to the retina,23 and respond rapidly with transient increases of intracellular calcium and protein expression.24 In mouse models, ablation of Müller cell glia from the developing mouse retina causes it to rip apart at the level of the ganglion cell layer in maturity.23 Therefore, the splitting of the retina that sometimes occurs in patients with glaucoma may stem from the microscopic changes that take place during a pathological rise in IOP, and vitreous fluid may accumulate through these weakened bridging structures.22
While peripapillary retinoschisis has been reported to spontaneously resolve,12,25,26 reports have also shown resolution of the lesion after intraocular pressure has been lowered through topical medication or via surgical procedures such as trabeculectomy.27–29 Anti-vascular endothelial growth factor injections may also help to resolve peripapillary retinoschisis, especially if subretinal fluid is present.18 Finally, pars plana vitrectomy (PPV) has also been shown to be an effective surgical option in cases where clear vitreomacular adhesions can be identified.9,25,28,30
Conclusion
This case reinforces the potential association between peripapillary retinoschisis and severe glaucoma. Several pathophysiological mechanisms have been proposed to explain the connection between these pathologies. Imaging with fundus photography and OCT should be obtained to confirm the presence of retinoschisis and document the severity of glaucoma, with treatment focused on lowering intra-ocular pressure through medical or surgical means.
References
- Lee EJ, Kee HJ, Han JC, Kee C. The Progression of Peripapillary Retinoschisis May Indicate the Progression of Glaucoma. Invest Ophthalmol Vis Sci. 2021 Feb 1;62(2):16.
- Hollander D, Barricks M, Duncan J, et al. Macular schisis detachment associated with angle-closure glaucoma. Arch Ophthalmol. 2005 Feb;123(2):270-2.
- Hwang Y, Kim Y, Kim H, et al. Effect of peripapillary retinoschisis on retinal nerve fibre layer thickness measurement in glaucomatous eyes. Br J Ophthalmol. 2014 May;98(5):669-74.
- Grewal DS, Merlau DJ, Giri P, et al. Peripapillary retinal splitting visualized on OCT in glaucoma and glaucoma suspect patients. PLoS One. 2017 Aug 23;12(8):e0182816.
- Batta P, Engel H, Shrivastava A, et al. Effect of partial posterior vitreous detachment on retinal nerve fiber layer thickness as measured by optical coherence tomography. Arch Ophthalmol. 2010 Jun;128(6):692-7.
- Kahook M, Noecker R, Ishikawa H, et al. Peripapillary schisis in glaucoma patients with narrow angles and increased intraocular pressure. Am J Ophthalmol. 2007 Apr;143(4):697-9.
- Zhao M, Li X. Macular retinoschisis associated with normal tension glaucoma. Graefes Arch Clin Exp Ophthalmol. 2011 Aug;249(8):1255-8.
- Tawara A, Miyamoto R, Tou N, et al. A classic temporal optic disc pit showing progression in the corresponding optic nerve fiber and visual field defects. Jpn J Ophthalmol. 2013 May;57(3):263-7.
- Yoshikawa T, Nishimura T, Minamino K, et al. A long-term follow-up of peripapillary retinoschisis with optic disc hypoplasia. Int Ophthalmol. 2013 Aug;33(4):425-8.
- Moreno-López M, González-López JJ, Jarrín E, Bertrand J. Retinoschisis and macular detachment associated with acquired enlarged optic disc cup. Clin Ophthalmol. 2012;6:433-6.
- Bayraktar S, Cebeci Z, Kabaalioglu M, et al. Peripapillary Retinoschisis in Glaucoma Patients. J Ophthalmol. 2016;2016:1612720.
- Lee EJ, Kim TW, Kim M, Choi YJ. Peripapillary retinoschisis in glaucomatous eyes. PLoS One. 2014 Feb 28;9(2):e90129.
- Kičová N, Bertelmann T, Irle S, et al. Evaluation of a posterior vitreous detachment: a comparison of biomicroscopy, B-scan ultrasonography and optical coherence tomography to surgical findings with chromodissection. Acta Ophthalmol. 2012 Jun;90(4):e264-8.
- Yonemoto J, Ideta H, Sasaki K, Tanaka S, Hirose A, Oka C. The age of onset of posterior vitreous detachment. Graefes Arch Clin Exp Ophthalmol. 1994 Feb;232(2):67-70.
- Shen Z, Duan X, Wang F, et al. Prevalence and risk factors of posterior vitreous detachment in a Chinese adult population: the Handan eye study. BMC Ophthalmol. 2013 Jul 16;13(1):33.
- Shao L, Xu L, You QS, et al. Prevalence and associations of incomplete posterior vitreous detachment in adult Chinese: the Beijing Eye Study. PLoS One.
- Hayreh SS, Jonas JB. Posterior vitreous detachment: clinical correlations. Ophthalmologica. 2004 Sep-Oct;218(5):333-43.
- Chuo JY, Lee TY, Hollands H, et al. Risk factors for posterior vitreous detachment: a case-control study. Am J Ophthalmol. 2006 Dec;142(6):931-7.
- Morita H, Funata M, Tokoro T. A clinical study of the development of posterior vitreous detachment in high myopia. Retina. 1995;15(2):117-24.
- Akiba J. Prevalence of posterior vitreous detachment in high myopia. Ophthalmology. 1993 Sep;100(9):1384-8.
- García-Bermúdez MY, Freude KK, Mouhammad ZA, et al. Glial Cells in Glaucoma: Friends, Foes, and Potential Therapeutic Targets. Front Neurol. 2021;12:624983.
- Fortune B, Ma KN, Gardiner SK, et al. Peripapillary Retinoschisis in Glaucoma: Association With Progression and OCT Signs of Müller Cell Involvement. Invest Ophthalmol Vis Sci. 2018 Jun 1;59(7):2818-2827.
- MacDonald RB, Randlett O, Oswald J, et al. Müller glia provide essential tensile strength to the developing retina. J Cell Biol. 2015 Sep 28;210(7):1075-83.
- Lindqvist N, Liu Q, Zajadacz J, et al. Retinal glial (Müller ) cells: sensing and responding to tissue stretch. Invest Ophthalmol Vis Sci. 2010 Mar;51(3):1683-90.
- Inoue M, Itoh Y, Rii T, et al. Spontaneous resolution of peripapillary retinoschisis associated with glaucomatous optic neuropathy. Acta Ophthalmol. 2015 Jun;93(4):e317-8.
- Dhingra N, Manoharan R, Gill S, et al. Peripapillary schisis in open-angle glaucoma. Eye (Lond). 2017;31:499–502.
- Pedruzzi NG, Ghirelli W, Cvintal V. Peripapillary retinoschisis and serous detachment of neurosensory retina after a non-penetrating deep sclerectomy. Rev Bras Oftalmol. 2018;77(6):356-9.
- Zumbro DS, Jampol LM, Folk JC, et al. Macular schisis and detachment associated with presumed acquired enlarged optic nerve head cups. Am J Ophthalmol. 2007;144:70–4.
- Woo R, Akil H, Koulisis N, et al. Sustained Resolution of Macular Retinoschisis After Trabeculectomy in a Patient With Progressive Glaucoma. J Glaucoma. 2017;26:e180-e6.
- Orazbekov L, Yasukawa T, Hirano Y, et al. Vitrectomy without gas tamponade for macular retinoschisis associated with normal-tension glaucoma. Ophthalmic Surg Lasers Imaging Retina. 2015;46:107–10.