Photo Essay and A Brief Report on New Rhegmatogenous Retinal Detachment Management

Summary: This brief report shows a fundus photo of a large retinal tear and contrasts the differences between pneumatic retinopexy (PnR), pars plana vitrectomy (PPV), and minimal gas vitrectomy (MGV) in rhegmatogenous retinal detachment (RRD) intervention.
Keywords: Rhegmatogenous retinal detachment; pneumatic retinopexy; minimal drainage vitrectomy; pars plana vitrectomy
Case Discussion
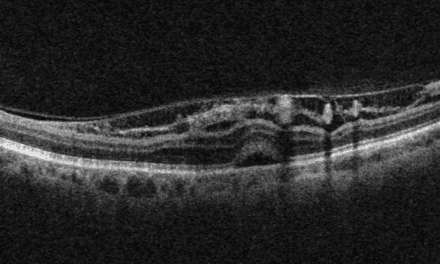
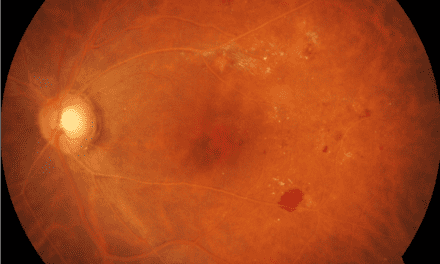
A 62-year-old myopic male presented after a minor motor vehicle accident with 14-day symptoms from a horseshoe tear and bullous macula-attached retinal detachment associated with a previously documented area of lattice degeneration in the left eye (Figure 1).

Figure 1. A superior retinal horseshoe tear and bullous macula-attached rhegmatogenous retinal detachment associated with lattice degeneration in the left eye
His presenting corrected visual acuity was 20/20 in the right eye and 20/100 in the left eye. He underwent a high-integrity retinal reattachment with pars plana vitrectomy, comprised of air-fluid exchange (AFX) and endolaser (EL) using long-acting 8% perfluoropropane (C3F8) (Figure 2). In addition, a phacoemulsification cataract extraction was performed before the RRD repair in a combined procedure.

Figure 2. One month status post pars plana vitrectomy
The surgical notes detailed the repair of a retinal horseshoe tear with secondary superior retinal detachment and inferior lattice degeneration using a vitrector to remove the peripheral vitreous, including vitreous traction over the tear and an area of inferior lattice degeneration in the attached retina. The inferior lattice was surrounded by endolaser, and subretinal fluid was drained through the retinal break with a soft-tipped cannula to flatten the retina. A small amount of loculated fluid was noted. The retinal tear was surrounded with multiple rows of endolaser photocoagulation. Another row of laser spots was applied 360 degrees to the peripheral retina. C3F8 gas was instilled through the infusion cannula, venting air through the supratemporal cannula. After removing the trocars, the wounds were self-sealing, and good intraocular pressure was confirmed. At one month and six months postoperatively, the retina was attached and the patient was asymptomatic.
Discussion
PIVOT Trial
The Pneumatic Retinopexy versus Vitrectomy for the Management of Primary Rhegmatogenous Retinal Detachment Outcomes Randomized Trial (PIVOT) concluded that pneumatic retinopexy (PnR) should be the first line treatment for rhegmatogenous retinal detachment (RRD) in patients meeting recruitment criteria.1
These criteria were: a single or group of breaks, one clock hour or less, above the eight and four o’clock meridian with additional breaks or lattice in the attached retina at any location.1 The results reported superior visual acuity, superior subjective visual function – as determined by the National Institute of Health visual function questionnaire – and superior vertical metamorphopsia scores with PnR procedures over PPV.1 Anatomic success was defined as a successful retinal attachment accomplished with a single procedure without a tamponade agent.1
Pneumatic Retinopexy
The Pneumatic Retinopexy procedure occludes the retinal break with an intravitreal gas bubble, provoking subretinal fluid reabsorption by the retinal pigment epithelium.5 Before the gas injection, the pneumatic retinopexy surgical process applies laser to all lattice degeneration and breaks in the attached retina.1 Twenty-four to 48 hours after gas injection, breaks in the detached retina are treated with cryotherapy or laser retinopexy.1 An anterior chamber paracentesis created to express ≥ 0.3 milliliters of fluid is followed by injection of ≥ 0.6 milliliters of short-acting 100 percent sulphur hexafluoride (SF6) expansile gas.1 A steamroller maneuver to expedite retinal reattachment pushes subretinal fluid (SRF) through the retinal break, protecting the macula from the risk of displaced SRF.1 The PnR technique—not widely utilized, is associated with a lower risk of retinal displacement compared to PPV.5
Pars Plana Vitrectomy and Minimal Gas Vitrectomy
Pars plana vitrectomy is the most common primary procedure for RRD among surgeons and it has excellent single-surgery anatomic success rates.1,3, The minimal drainage vitrectomy procedure or minimal gas vitrectomy (MGV) modifies the standard pars plana vitrectomy with gas, decreasing the incidence of retinal misalignment and long-term symptoms.3 Compared to conventional pars plana vitrectomy, the MGV technique employs minimal subretinal fluid drainage and uses a smaller gas tamponade. Precise patient positioning and the PnR steamrolling technique to express subretinal fluid allow the RPE pump mechanism to reabsorb the remaining fluid aiding in natural photoreceptor alignment accuracy.3 The repair is followed by the application of laser retinopexy to the newly attached retina on postoperative day one.3 In addition to high-integrity retinal reattachment outcomes, the minimal gas vitrectomy may reduce retinal displacement at rates consistent with pneumatic retinopexy.3
References
-
- Hillier RJ, Feldeli T, Berger AR, et al. The Pneumatic Retinopexy versus Vitrectomy for the Management of Primary Rhegmatogenous Retinal Detachment Outcomes Randomized Trial (PIVOT). Ophthalmology. 2019;126(4):531-539
- Ryan EH, Ryan CM, Forbes NJ, et al. Primary Retinal Detachment Outcomes Study Report Number 2. Am Acad Ophthalmol. 2020;127(8) 1077-1085
- Muni RH, Felfeli T, Figueiredo F, et al. Minimal Gas Vitrectomy Technique for Reducing Risk of Retinal Displacement Following Rhegmatogenous Retinal Detachment Repair. Retin Cases Brief Rep. 2022; 16(6): 681-684
- Brosh K, Francisconi CL, Qian J, et al. Retinal displacement following pneumatic retinopexy vspars plana vitrectomy for rhegmatogenous retinal detachment. JAMA Ophthalmol.2020;138:652-659
Leslie R. Wilderson, OD, FAAO, Dipl AAO, graduated from the Nova Southeastern University College of Optometry, completed a Primary Eyecare Residency, and is board certified in medical optometry (ABCMO). Dr. Wilderson is an American Academy of Optometry Fellow, American Academy of Optometry Diplomate in the Comprehensive Eye Care Section, and Journal of Medical Optometry Editorial Board member. She is on the optometry staff at the Northeast Ohio VA and serves in the Air Force Reserve.